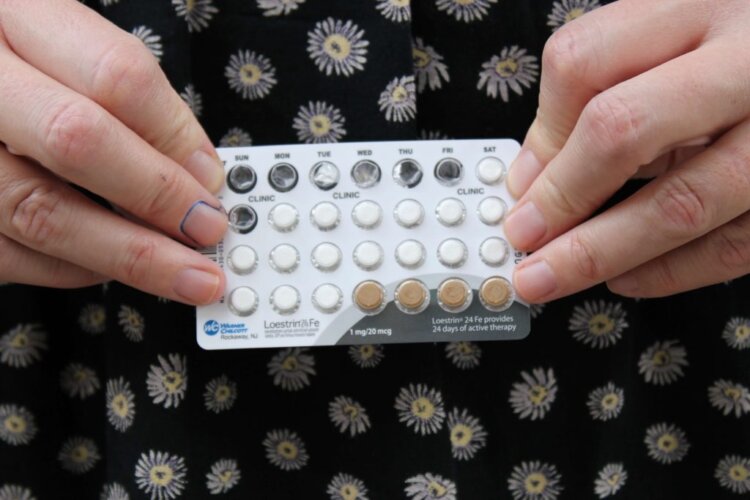
Of the twenty or more birth control options currently available, upwards of 16 of them are for women, and just three of them are for men. Women have an ever-expanding array of synthetic hormone-based choices, from the pill to the hormonal IUD to the shot. Men have condoms, vasectomy, and the pullout method.
When the birth control pill was first released in 1961 it aligned well with the feminist cause that women be “in control” of their reproductive abilities. Yet, as the years rolled on, it’s become clear that this control comes at a cost to women’s health and well-being in the form of side effects. The feminist women’s health movement was founded by Barbara Seaman, who saw prescribing the birth control pill to prevent pregnancy as “tinkering with nuclear bombs to fight off the common cold.” She understood that the risks of this method would not outweigh the benefits for many women. Where women once desired the freedom the pill offered, they may now feel the expectation to use hormonal birth control is an unfair burden.
The further we’ve moved away from the advent of the pill, the further we’ve gotten away from the facts of our fertility. Because women are only able to get pregnant on six days per menstrual cycle, to have women take such a powerful medication every single day to prevent ovulation, which occurs on just two days per menstrual cycle, seemed like overkill to Seaman.
A woman usually has three decades of fertile years, between puberty and menopause. Men, however, are fertile every single day and can impregnate women from a very early age and well into their old age, essentially their whole lives. A woman, once pregnant, cannot get pregnant again for a year, usually longer. When a man gets a woman pregnant, he can get another woman pregnant the next day, and so on, without end. This is another reason why men should be shouldering more of the burden when it comes to contraception.
And while it’s true that only women get pregnant, they never do so without the presence of sperm – so why shouldn’t the medical community better understand that men “need” birth control as much as women do, and focus a more equal share of their research efforts in developing contraception methods for men?
Use of the most effective options currently available to men – condoms and vasectomy – is on the decline. Condom use has dropped steeply since the early 2000s. Vasectomy rates are down by as much as 64% in the last ten years. It’s important to note that while vasectomy is a relatively simple outpatient procedure, as is its reversal, which if done within a few years can be up to 70% successful in restoring fertility; female sterilization is a more invasive surgery, higher risk, with reversal usually not an option, and three times as many women get medically sterilized in a given year than men get vasectomies.
Although men do not have as many options for birth control as women, they are not using the options available very enthusiastically. And this is despite the fact that condoms, in addition to helping to prevent pregnancy, are the only way to prevent sexually transmitted diseases or infections. (And for women, it is much easier to get a sexually transmitted disease or infection than it is to get pregnant – men should be more conscientious about using condoms for both these reasons.)
When another round of research is released suggesting the promise of a new male contraceptive (which happens about every six months, it seems), it is usually met with optimism and positive speculation. However, when just last week we received news of research into a hormone-based male contraceptive injection, published by the Journal of Clinical Endocrinology and Metabolism, women had a very different reaction. The headlines conveyed a barely suppressed anger that, despite some 60 years of investigation into hormonal birth control for men, there’s still not a single one available on the market. And the reason why, which researchers and other experts gave, was met with sarcasm and calls of sexism: because the side effects of a hormonal contraceptive injection for men are too serious and occur too frequently. What are these upsetting side effects? They are a high rate of mood disorders, acne, hypertension, pain and other side effects very similar to those women experience on their hormonal birth control options.
This particular study was published hot on the heels of another significant paper, just weeks prior from the University of Copenhagen, which revealed many female hormonal contraceptives (the pill, hormonal IUD, patch, ring) increased the risk of depression for women.
What became clear after the publication of these articles is that the only reason we do not have male hormonal birth control is because it would do to men the exact same thing it has done to women for decades already.
Previously women’s experiences of depression and anxiety on the pill were dismissed as psychosomatic or the result of “rumor and gossip.” Doctors were advised to not even inform women of the possibility they might experience these side effects.
And while male hormonal birth control won’t be approved for use because of these side effects, women needed the study from the University of Copenhagen for any kind of vindication of their personal experience and acknowledgement from the medical establishment that, yes, the pill might cause depression (although it was mostly a begrudging acknowledgement).
Although some women might want the general male population to experience these side effects for themselves, in the name of equality and, perhaps, to elicit anger for what women have been expected to suffer through, others suggested we focus on getting researched non-hormonal options for men released, like Vasalgel. But underlying every woman’s response is the demand that the side effects we experience be taken as seriously and received with as much concern as the medical establishment seems to have for the men’s side effects.
There are non-hormonal options available to women – the copper IUD, diaphragm, cervical cap , and new technology that makes it ever-easier to practice the fertility awareness method. But within this structure of sexism that refuses to balance the burden of preventing pregnancy, ignores the facts of our fertility, and dismisses the health and well-being of women, these choices are kept out of reach.
Shared responsibility can start today – with men using the options they already have available to them and not pressuring women to use hormonal birth control. But it will become a reality only when we truly care about women.
 Holly Grigg-Spall is the author of “Sweetening the Pill: Or How We Got Hooked On Hormonal Birth Control.” She is a consulting producer on the documentary inspired by her book that is currently in production, with director Abby Epstein and executive producer Ricki Lake. Holly is a freelance writer who currently works as a writer and consultant for two women’s health-centric companies – Daysy and FLO Living – as well as producing articles for the likes of the Guardian and Marie Claire. Holly’s work has recently featured in Vogue, the Washington Post, Broadly, the BBC and CBC. You can learn more on her website.
Holly Grigg-Spall is the author of “Sweetening the Pill: Or How We Got Hooked On Hormonal Birth Control.” She is a consulting producer on the documentary inspired by her book that is currently in production, with director Abby Epstein and executive producer Ricki Lake. Holly is a freelance writer who currently works as a writer and consultant for two women’s health-centric companies – Daysy and FLO Living – as well as producing articles for the likes of the Guardian and Marie Claire. Holly’s work has recently featured in Vogue, the Washington Post, Broadly, the BBC and CBC. You can learn more on her website.


Grok Nation Comment Policy
We welcome thoughtful, grokky comments—keep your negativity and spam to yourself. Please read our Comment Policy before commenting.